What is Hipec Surgery?

What is Hipec Surgery?
HIPEC in ovarian cancer
However, even in patients with complete cytoreductive surgery, the recurrence rate of the disease is high (above 50%), which is associated with poor survival rates, especially in patients with peritoneal disease.
Postcytoreductive surgery intraperitoneal chemotherapy in combination with intravenous chemotherapy has been shown to have improved survival results in patients treated with intraperitoneal chemotherapy.
US National Cancer Institute advocates the use of postoperative IP chemotherapy in patients with stage III ovarian cancer after optimal cytoreduction.
Large scientific trials have shown that the survival for the patients with ovarian cancer is longest with the use of intraperitoneal chemotherapy than any other treatment so far and also the risk of death is reduced with each cycle of intraperiotneal chemotherapy received.
HIPEC, developed on the basis of intraperitoneal chemotherapy, has been gaining popularity in the last decade as an effective treatment option for the microscopic residual disease remaining behind in the abdomen after complete cytoreductive surgery.
Malignancies with great tendency to spread to the peritoneum, those sensitive to systemic chemotherapy, and those with resectable disease of the peritoneum would be more likely to benefit from HIPEC, and it has already established itself as an effective treatment option in peritoneal surface malignancies such as pseudomyxoma, colon cancer with peritoneal dissemination and peritoneal malignant mesothelioma.
Rationale of HIPEC in ovarian cancer
Systemic metastases are generally observed in late stages of the natural history of ovarian cancer. The fact that the disease remains confined for long periods of time in the peritoneal cavity and the low penetrance of systemic chemotherapy into the peritoneal cavity, justifies the implementation of local therapy in the form of HIPEC acting directly on the source of the problem.
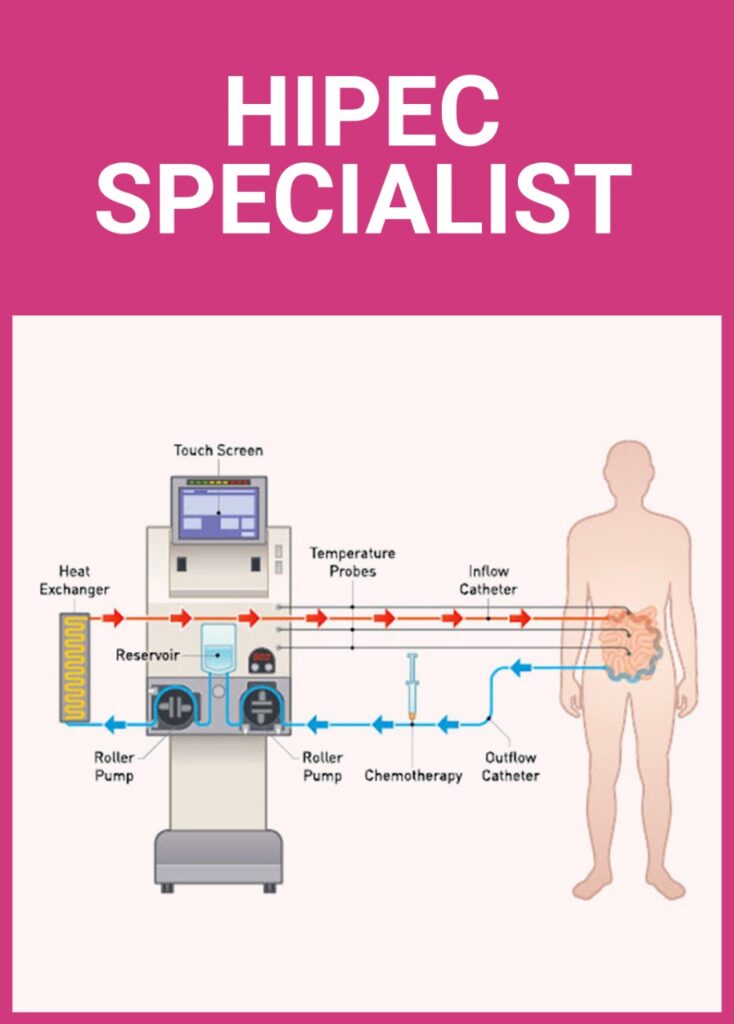
In theory, the HIPEC treatment allows the effective treatment of the microscopic residual disease cells after cytoreductive surgery, by mechanical (continuous flow of the perfusion solution), physical (heat) and chemotherapy cytotoxicity related measures.
Taking advantage of the peritoneum-plasma barrier, it is possible to achieve very high drug concentrations in the peritoneal cavity with minimum plasma drug concentrations, thereby reducing the risk of systemic toxic side effects of chemotherapy.
During HIPEC, the most active drugs allow peritoneum/plasma ratios that range from 20 times, as it is seen with platinums (cisplatin and carboplatin) and up to 1000 times as seen in taxanes (paclitaxel, docetaxel).
In addition to the cytotoxic effects of chemotherapy, the use of hyperthermia is another key factor of HIPEC. Hyperthermia on its own has anticancer effects and has also demonstrated a positive combined antitumor effects of chemotherapy drugs, by allowing greater penetration of the drug into the tumor.
The mechanism of action of hyperthermia on tumor cells could be related to the alterations of the mechanisms of DNA repair, protein denaturation, and inhibition of the oxidative metabolism that occur in the tumor microenvironment, leading to an increase in the acidity of the surroundings, lysosomal activation and increased
cell death.
Rationale of HIPEC in ovarian cancerScientific evidence and clinical results
Emerging evidence suggests that HIPEC with cytoreductive surgery (CRS) shows a survival benefit over CRS alone for patients with epithelial ovarian carcinoma (EOC).
In a systematic review and meta-analysis of 9 comparative studies and 28 studies examining HIPEC and CRS for primary and/or recurrent ovarian cancer, D.L. Morris et al. concluded that the addition of HIPEC to CRS and chemotherapy improves overall survival rates for both primary and recurrent ovarian cancer. Morbidity and mortality rates were similar.
Results of the phase 3 randomised multicentre trial of HIPEC with interval debulking surgery after neo-adjuvant chemotherapy for stage III epithelial ovarian cancer from Netherlands were presented in ASCO 2017 annual meeting.
They concluded that the addition of HIPEC to interval cytoreductive surgery is well tolerated and improves recurrence free and overall survival in patients with stage III epithelial ovarian cancer.
CRS with HIPEC procedure may entail multiple peritoneal and visceral resections to achieve complete cytoreduction, as well as the local and systemic adverse effects of HIPEC, give rise to concerns with respect to the health-related Quality of Life-HRQoL of patients undergoing this major procedure.
In a systematic review of the studies assessing quality of life in these group of patients using validated questionnaires, it was demonstrated that although overall QoL scores drop in the immediate postoperative period, at an average of 3 months post procedure they recover to 80%e100% or even exceed baseline values. Furthermore, between 6 and 12 months postoperatively, overall QoL is improved in survivors compared to pre-operative status.
